|
Over fifty million Americans have allergies and thirty-two million have food allergies. You probably know one of those people or are one yourself. But why does allergic reaction occur? An allergic reaction occurs when your immune system overreacts to a food or a substance in a food, thus identifying it as a danger and triggering a protective response. Symptoms of a food allergy can range from mild to severe, with the most severe allergic reaction being anaphylaxis. During an anaphylaxis shock, Epinephrine may be life-saving if administered to a person as quickly as possible. However, in minor cases, prescribed antihistamines such as diphenhydramine (Benadryl) may help reduce symptoms. What is the science behind an EpiPen? The first-line treatment for anaphylaxis is epinephrine (adrenaline). It is available by prescription in an auto-injector named EpiPen. Epinephrine works by reversing the symptoms of anaphylaxis. For example, when you inject an Epipen on the thigh, a person's blood pressure decreases during an anaphylactic reaction because the blood vessels relax and dilate however the epinephrine causes the blood vessels to constrict, thus raising blood pressure. Epinephrine is the synthetic form of the naturally occurring sympathomimetic amine with vasoconstricting (constriction of blood vessels thus raising blood pressure), intraocular pressure-reducing, and bronchodilating activities (An expansion of the air passages through the bronchi of the lungs). Additionally, Epinephrine elevates the blood sugar levels by increasing the hydrolysis of glycogen to glucose in the liver, and at the same time, it begins the breakdown of lipids in adipocytes (a cell specialized for the storage of fat). In all, Epinephrine has a suppressive effect on the immune system. What is the science behind antihistamines? Antihistamines reduce or block histamines, therefore they can stop allergy symptoms. It works well to relieve symptoms of different types of allergies, including seasonal, indoor, and food allergies. Antihistamines block H1 histamine receptors. They replace histamine at receptor sites (proteins that receive signals for a cell) at which it becomes bound in various susceptible tissues. Thus it prevents histamine-triggered reactions under conditions like food allergies. In terms of the difference between antihistamines and epinephrine, it is essential to note that epinephrine is not a long-term medication for allergies, and should not be a substitute for allergy medications like antihistamines. By: Vasundhara Kulkarni
0 Comments
Around 32 million Americans are currently living with food allergies that can make everyday grocery shopping a difficult task. And with the onset of COVID-19 leaving store shelves across the nation devoid of most foods, the task of preparing food becomes even more dire for those who suffer from food allergies.
For those who have food allergies and other dietary restrictions, grocery shopping is not just a matter of picking the freshest or the yummiest ingredients on the shelves— it’s a serious matter of safety and health. In the most severe cases, it can be a matter of life and death. Anywhere from around 1 to 5% of Americans are believed to suffer from anaphylaxis, a severe allergic reaction that can cause potentially life-threatening effects within minutes of contact with an allergen. Other dietary restrictions such as the gluten-free diet required by those with celiac disease also require much more selectivity when it comes to purchasing food— selectivity that becomes difficult when shelves are empty due to increased buying from the ongoing coronavirus pandemic. COVID-19 has had especially devastating effects on our community in New Jersey. As of Friday, May 8th 2020, the state has seen over 130,000 confirmed cases and nearly 9,000 deaths due to the virus. Grocery stores have continued to witness overwhelming demand for products such as toilet paper, disinfectant, and produce, resulting in many stores instating a limit on purchases in order to fight hoarding. Luckily, there are ways to help. Lisa G. Gable, the CEO of the nonprofit Food Allergy Research & Education, recommended that shoppers without food allergies exercise caution when making choices about what to buy at the supermarket. She asked that shoppers consider others’ dietary restrictions when purchasing items like soy milk and gluten-free foods which are necessary for many who need to eat those to survive. For those with food allergies, Kids With Food Allergies recommends that families take greater precautions when cooking due to the newfound proximity of family members who may have different dietary restrictions. They also recommend shopping strategically by minimizing visits to the store and looking for local grocery delivery services. This will be a difficult fight, but working together as a community, we can get through this. Here at Nourish, we would like to ask everyone to be mindful of what they purchase and keep other shoppers in mind— especially those who may not have the luxury of eating whatever is left on the shelves. Though this pandemic presents uncharted territory for us as a nation, we strongly believe in the fight to overcome this challenge together. Remember to follow social distancing guidelines and stay safe everyone! By: Michelle Liu Introduction
When it comes to food allergies, pets are not too different from humans. Although they are less common, around 10% of dogs and 13% of cats have food allergies. The most common allergies in pets stem from beef, chicken, dairy, and fish. They could be caused by both genetic predispositions and environmental effects, especially if they were exposed to antibiotics at an early age. Pets cannot develop allergies for foods they have not been exposed to. As they are less common, many people do not know what to do when their pet has an allergic reaction to the food they eat, but worry not! Symptoms The most common symptoms for dogs include chronic ear inflammation, gastrointestinal problems (including diarrhea, constipation, and vomitting), and anal fissures or itches. Cats display many of the same symptoms, but are much more prone to itchy skin, which can lead to wounds. In less common pets such as hamsters or other rodents, violent bursts of sneezing has been observed. These symptoms occur almost immediately after the pet has eaten something that it should not have. They may sometimes subside on their own, but most likely require some form of medical attention. Treatment Options As with most people, allergies last for a lifetime in pets. The best options for relieving your pet of its allergies is to simply not feed them the food that makes them allergic, and avoid dog and cat food packets that may induce allergies. Making your pet go vegetarian is not recommended, as it deprives your pet of the essential nutrients it needs. If your dog or cat were to have an allergic reaction to any of the food it eats, be sure to give it the proper medication. Antihistamines (excluding OTC) are known to work especially well. Sentry and Petlab are renowned for their medications for pet allergies. If they are not available, most over the counter medicine in moderation is known to work as well. This includes Claritin, Benadryl, and Zyrtec. Avoid Tylenol and Ibuprofen, as they are not safe for pets. If the condition of your pet gets worse, be sure to visit your vet. Allergy Friendly Options There are many companies that provide allergy friendly pet food. With any pet food, however, make sure to read the labels and nutritional facts. Here are a few companies can try:
For more information on OTC medications for pet allergies, you can visit https://yourdogadvisor.com/otc-pain-meds-for-dogs/ By: Shravya Harish With National Decision Day having just passed on May 1, high school seniors across the country have now committed to their future colleges or universities. Naturally, these soon-to-be college students have been thinking about and planning how they will begin their college experience. With students with food allergies, however, this planning sometimes looks a little bit different. Nonetheless, with some extra caution and preparation, these students will be able to experience the full college experience with their peers.
By: Nami Jain All across America, Thanksgiving is celebrated as a time of love, appreciation, and gathering. Unfortunately, many families across the nation cannot afford to buy adequate food supplies year round — let alone for Thanksgiving. The situation is even more troubling for individuals who also experience medical dietary restrictions; allergen-free food is often even more expensive and inaccessible.
What is Nourish America doing about it? This Thanksgiving, Nourish America is helping all families in the local area spend time with their families without having to worry about getting food on the table. We are excited to announce that we will be hosting an allergy-friendly food drive at the ShopRite in South Plainfield, NJ! How can I get involved? There are many ways for you to get involved in helping members of your community! The easiest is by participating in food drives — you simply have to buy an extra canned or boxed good when you stop by the grocery store. Make sure to contribute to our food drive by buying an allergen-free food and dropping it in the box at the entrance of ShopRite. You can also spread awareness by handing out our food drive flyers or simply by talking to others that you interact with on a day-to-day basis. Spreading awareness will help more people join the cause and understand the severity of the issue, and possibly even donate. You can also consider volunteering at your local food bank or hosting your own food drive. Although this requires a larger commitment of time and effort, it will really make a difference and allow significantly more people to enjoy Thanksgiving with allergy-friendly food on their plates. And finally, use your creativity and skills to come up with ideas of your own! There are so many ways to give back to the community and utilize your talents at the same time. Happy Thanksgiving! By Nami Jain Thanksgiving is a holiday in which people gather to celebrate all that they have to be thankful for: family, friends, good health, to name a few. However, not everyone is able to celebrate Thanksgiving with food on their table.
The USDA defines food insecurity as “a household-level economic and social condition of limited or uncertain access to adequate food.” In 2018, 14.3 million American households were classified as having food insecurity. This is a staggering number which becomes even more worrisome because 12 million American children live in food-insecure homes today. Food insecurity can have a profound impact on society and public health. People with food insecurity sometimes live in “food deserts” or areas where it is difficult to buy affordable and fresh foods. In such areas, supermarkets are few and far between, while fast food restaurants are numerous. Thus, it is no surprise that food insecurity is associated with a rise in obesity in at least twelve states. People who live in food deserts often resort to eating inexpensive, calorically dense foods with poor nutritional value. To solve food insecurity in America, a nonprofit organization called the Fair Food Network in Detroit, MI (one of the nation’s top food deserts) has come up with a solution: the Double Up Food Bucks program. Under this initiative, Michigan Supplemental Nutrition Assistance Program (SNAP) participants get double value for every SNAP dollar they use to buy fresh fruits and vegetables at certain grocery stores. Indeed, the Double Up program is not a panacea for food insecurity: more supermarkets need to be built in food deserts and public transportation improved so that people can reach them. But it shows how states can incentivize and support people with food insecurity to access healthful foods. Another organization working to end food insecurity is the Community Food Bank of New Jersey. As the state’s largest anti-hunger and anti-poverty organization, CFBNJ provides millions of meals annually to New Jerseyans living in hunger. Nourish America is proud to announce that the allergen-free donations from our 2019 Thanksgiving Food Drive, in collaboration with ShopRite, will be donated to the CFBNJ in Hillside, NJ so that they can continue giving throughout the holiday season and beyond. Sources: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5230819/ CFBNJ Official Website: https://www.cfbnj.org/ By Shreya Shivakumar The immune system is the human body's extremely powerful reaction system that thwarts bodily invaders like germs, viruses, and bacteria. Usually, it does wonders to fight dangerous infections and diseases with reactions like swelling and fever — however, it can sometimes mistake harmless objects for truly threatening ones, causing an allergic reaction to occur.
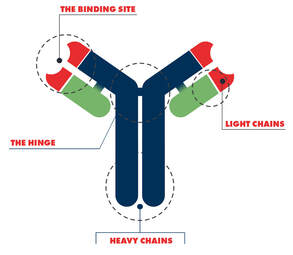
While almost anything can trigger an allergic reaction, from dust mites to pollen, one of the most common causes is a specific type of food, most commonly peanuts, tree nuts, and shellfish. It is estimated that about 4-6% of Americans have a type of food allergy, and for some, dietary restrictions can make it extremely difficult to find a proper meal. Today, we're going to investigate more closely the relationship between food allergies and the immune system. You may already be familiar with what an antibody is — a Y-shaped protein in the blood that can bond to a specific kind of particle in order to neutralize it by impeding it from functioning or by allowing another immune system cell to swallow it. These immunoglobulins are usually used to fight harmful pathogens — however, for people with food allergies, antibodies (called IgE in this case) develop in order to "fight" innocuous food particles. When this bonding occurs between the allergen and the IgE, mast cells release a hormone called histamine that causes allergic symptoms like itching, sneezing, swelling, and a runny nose that normally fight dangerous bacteria but are now unleashed against something as harmless as a walnut. Surprisingly, allergies occur more often in those who have primary immunodeficiencies, or a sub-optimally performing immune system. Because PIs often only affect a part of the immune system, the rest of the system will not be regulated as well and bad reactions can be exaggerated due to the lack of control and stability within the body. Additionally, exposure to bacteria as well as the medication to fight them can negatively affect the immune system as a whole and worsen the reactions as well. PIs and food allergies could also share a specific genetic cause, making them inherently interlinked. This can also make it more difficult to identify the cause behind certain symptoms — is my runny nose due to an allergy, a cold, a weak immune system, or all three? Even medical professionals can be confused by the variety of interrelated symptoms and infections that may result from an assortment of immune system issues, from allergies to a PI. Scientific and medical research continues to investigate these relationships and the complex causes behind food allergies. If you think you may be suffering from a food allergy, we recommend keeping an eye out for any possible clues, but don't be too quick to diagnose yourself — always go to a medical professional first if you have any questions or doubts. Happy early Thanksgiving from us to you at Nourish America! By Michelle Liu Food allergies are on the rise, and it is extremely important to be aware of the procedures in dealing with them, especially in children. Allergies occur when an individual’s immune system identifies a particular food as foreign and attacks its proteins, known as allergens. A chemical, called histamine, is released due to exposure to the allergen, causing the reaction. Depending on the child’s sensitivity to the allergen, the allergic reaction can range anywhere from itching to possibly fatal. There are approximately 32 million Americans with food allergies, with 5.6 million of those under 18 years old. Peanut or tree nut allergies in particular in children have approximately tripled in the US between 1997 and 2008. Common food allergiesThese are the top 8 allergies to look out for in children:
Symptoms of an allergic reaction
Why food allergies are on the riseAlthough doctors have not yet pinpointed why children's food allergies are increasing, they have come up with theories regarding the cause of this change:
Helping children with food allergiesThere are many ways to help your child and family manage food allergies.
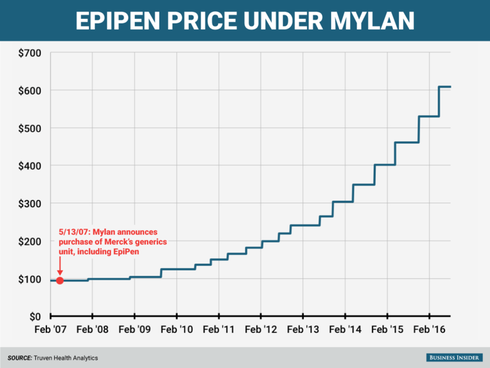
By Sriya Chinthalapudi Epinephrine is a life-saving drug used to provide rapid relief for patients who suffer from anaphylaxis. During a severe allergic reaction, the patient’s airways start to close. The EpiPen is epinephrine in an auto-injector form. EpiPens deliver epinephrine, or adrenaline, to make the patient’s heart beat faster and open up the airways to allow breathing. The EpiPen has been available in the US since 1987, where it is available in two doses: 0.3 mg for adults and 0.15 mg for children. In 2007, global pharmaceutical company Mylan bought the EpiPen from the Merck Group, its competitor. Since then, the price of a two-pack of Epipens has increased by over 500%, currently sitting at over $600.
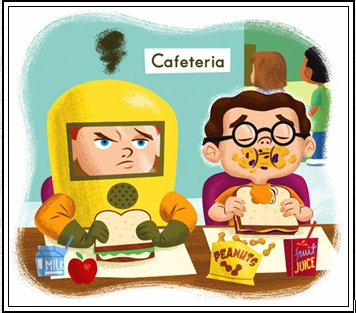
How can epinephrine, which costs less than $1 a milliliter, be sold for hundreds of dollars? Some argue that the inflated price of the drug can be traced back to its relatively short expiry date or convenient injecting system. Yet others attribute the skyrocketing costs to Mylan’s near-monopoly on the device. Nevertheless, over 3.6 million prescriptions for the EpiPen were written in 2015. After this drastic upsurge in EpiPen prices, many families were unable to guarantee that they would have EpiPens for their children with food allergies. Faced with public backlash, Mylan announced that it would offer a $300 “savings card” to buy a two-pack of EpiPens. While the company insisted that this discount would reduce the drug’s price by 50%, it only applied to patients with commercial insurance. The price would remain unchanged for patients with government insurance programs like Medicare or Medicaid or no insurance at all. Unable to afford Mylan’s EpiPen, many patients began to search for viable and cost-effective alternatives. Prescriptions to EpiPen alternatives such as Adrenaclick jumped by about 9% in January 2017 but then stagnated. Doctors could not confidently switch from prescribing alternatives because of their more difficult injecting systems. Furthermore, the FDA, citing insufficient evidence, has stated that it does not consider EpiPen and Adrenaclick to be therapeutically equivalent to one another. Mylan introduced a generic version of the EpiPen in December 2016, and Teva Pharmaceuticals followed with its own FDA approved version in August 2018; however, both these generics cost about $300 for a two-pack of epinephrine auto-injectors. Additionally, there has been a supply shortage of EpiPens since May 2018 due to problems at Pfizer’s manufacturing plants. This has prompted the FDA to extend the EpiPen’s expiry date by four months to ensure patients have access to the drug while the issues are being fixed. For families that rely on the EpiPen for their food-allergic children, there is no end in sight. They will have to empty their pockets for a generic alternative to this essential medication- that is, of course, if they are lucky enough to get their hands on it. By Shreya Shivakumar What is a food allergy? A food allergy occurs when the body has a specific immune response to foods. Some reactions can be severe and life-threatening, especially for children. Eight food groups account for 90% of serious allergic reactions in the US such as milk, fish, eggs, shellfish, wheat, peanuts, soy, and peanuts. In a typical classroom of 25 students, at least one student is likely to be affected by food allergies. How can we manage food allergies in schools? As a responsibility of a parent, guardian or school official, there are a plethora of ways to manage food allergies in schools. One of the first things to do is to make sure school officials and nurses are aware of the allergies a child possesses and provide necessary medication. Next, administrators need to ensure appropriate storage and administration of epinephrine. Most schools contain a stock of epinephrine auto-injectors, which was enforced by the School Access to Emergency Epinephrine Act, signed by President Obama in 2013. Another way to manage food allergies in schools is by designating allergy-safe seating areas during lunch to avoid reactions. Teachers should not allow food sharing for children who they know have allergies and encourage hand washing after handling food. For example, washing surfaces on which food has been eaten with wipes or spray cleaners are effective at removing peanut protein from surfaces. Another method is keeping “safe snacks” in a classroom for unplanned events is useful just in case the child’s lunch accidentally becomes contaminated. In environments where children are unable to bring lunch from home every day, posting lunch menus beforehand allows parents to identify unsafe meal offerings and plan accordingly for their child’s meals. Training food service personnel on allergy issues such as avoiding cross-contact with food preparation is a suggested requirement. All in all, the idea of promoting food allergy safety in schools requires collaborative efforts of parents, students, and staff.
By Vasundhara Kulkarni |
Details
Archives
May 2021
Categories |
Powered by
 Create your own unique website with customizable templates.
Create your own unique website with customizable templates.
 Create your own unique website with customizable templates.
Create your own unique website with customizable templates.









 RSS Feed
RSS Feed