|
Food allergies are on the rise, and it is extremely important to be aware of the procedures in dealing with them, especially in children. Allergies occur when an individual’s immune system identifies a particular food as foreign and attacks its proteins, known as allergens. A chemical, called histamine, is released due to exposure to the allergen, causing the reaction. Depending on the child’s sensitivity to the allergen, the allergic reaction can range anywhere from itching to possibly fatal. There are approximately 32 million Americans with food allergies, with 5.6 million of those under 18 years old. Peanut or tree nut allergies in particular in children have approximately tripled in the US between 1997 and 2008. Common food allergiesThese are the top 8 allergies to look out for in children:
Symptoms of an allergic reaction
Why food allergies are on the riseAlthough doctors have not yet pinpointed why children's food allergies are increasing, they have come up with theories regarding the cause of this change:
Helping children with food allergiesThere are many ways to help your child and family manage food allergies.
By Sriya Chinthalapudi
1 Comment
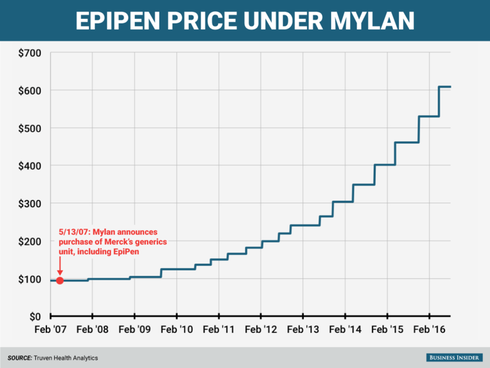
Epinephrine is a life-saving drug used to provide rapid relief for patients who suffer from anaphylaxis. During a severe allergic reaction, the patient’s airways start to close. The EpiPen is epinephrine in an auto-injector form. EpiPens deliver epinephrine, or adrenaline, to make the patient’s heart beat faster and open up the airways to allow breathing. The EpiPen has been available in the US since 1987, where it is available in two doses: 0.3 mg for adults and 0.15 mg for children. In 2007, global pharmaceutical company Mylan bought the EpiPen from the Merck Group, its competitor. Since then, the price of a two-pack of Epipens has increased by over 500%, currently sitting at over $600.
How can epinephrine, which costs less than $1 a milliliter, be sold for hundreds of dollars? Some argue that the inflated price of the drug can be traced back to its relatively short expiry date or convenient injecting system. Yet others attribute the skyrocketing costs to Mylan’s near-monopoly on the device. Nevertheless, over 3.6 million prescriptions for the EpiPen were written in 2015. After this drastic upsurge in EpiPen prices, many families were unable to guarantee that they would have EpiPens for their children with food allergies. Faced with public backlash, Mylan announced that it would offer a $300 “savings card” to buy a two-pack of EpiPens. While the company insisted that this discount would reduce the drug’s price by 50%, it only applied to patients with commercial insurance. The price would remain unchanged for patients with government insurance programs like Medicare or Medicaid or no insurance at all. Unable to afford Mylan’s EpiPen, many patients began to search for viable and cost-effective alternatives. Prescriptions to EpiPen alternatives such as Adrenaclick jumped by about 9% in January 2017 but then stagnated. Doctors could not confidently switch from prescribing alternatives because of their more difficult injecting systems. Furthermore, the FDA, citing insufficient evidence, has stated that it does not consider EpiPen and Adrenaclick to be therapeutically equivalent to one another. Mylan introduced a generic version of the EpiPen in December 2016, and Teva Pharmaceuticals followed with its own FDA approved version in August 2018; however, both these generics cost about $300 for a two-pack of epinephrine auto-injectors. Additionally, there has been a supply shortage of EpiPens since May 2018 due to problems at Pfizer’s manufacturing plants. This has prompted the FDA to extend the EpiPen’s expiry date by four months to ensure patients have access to the drug while the issues are being fixed. For families that rely on the EpiPen for their food-allergic children, there is no end in sight. They will have to empty their pockets for a generic alternative to this essential medication- that is, of course, if they are lucky enough to get their hands on it. By Shreya Shivakumar What is a food allergy? A food allergy occurs when the body has a specific immune response to foods. Some reactions can be severe and life-threatening, especially for children. Eight food groups account for 90% of serious allergic reactions in the US such as milk, fish, eggs, shellfish, wheat, peanuts, soy, and peanuts. In a typical classroom of 25 students, at least one student is likely to be affected by food allergies. How can we manage food allergies in schools? As a responsibility of a parent, guardian or school official, there are a plethora of ways to manage food allergies in schools. One of the first things to do is to make sure school officials and nurses are aware of the allergies a child possesses and provide necessary medication. Next, administrators need to ensure appropriate storage and administration of epinephrine. Most schools contain a stock of epinephrine auto-injectors, which was enforced by the School Access to Emergency Epinephrine Act, signed by President Obama in 2013. Another way to manage food allergies in schools is by designating allergy-safe seating areas during lunch to avoid reactions. Teachers should not allow food sharing for children who they know have allergies and encourage hand washing after handling food. For example, washing surfaces on which food has been eaten with wipes or spray cleaners are effective at removing peanut protein from surfaces. Another method is keeping “safe snacks” in a classroom for unplanned events is useful just in case the child’s lunch accidentally becomes contaminated. In environments where children are unable to bring lunch from home every day, posting lunch menus beforehand allows parents to identify unsafe meal offerings and plan accordingly for their child’s meals. Training food service personnel on allergy issues such as avoiding cross-contact with food preparation is a suggested requirement. All in all, the idea of promoting food allergy safety in schools requires collaborative efforts of parents, students, and staff.
By Vasundhara Kulkarni Anaphylaxis is a generalized term for a severe reaction to an allergen that may be fatal if left untreated. Epinephrine, more commonly referred to as adrenaline, may be life-saving if administered to a person experiencing an anaphylactic reaction as quickly as possible. What is anaphylaxis?Anaphylaxis is a severe allergic reaction that can happen within seconds of exposure to an allergen, with peanuts and dairy being popular examples. But what makes someone allergic to these seemingly inoffensive substances? People who are allergic to these substances are allergic because their bodies respond to them as if they were infections. Our bodies are designed to attack foreign antigens and kill them, which results in the typical immune response to fever or inflammation. When your body detects that harmless substances are the equivalent to a foreign flu virus or bacteria, you are going to experience an unneeded immune response every time you come in contact with these substances. Anaphylaxis is a more severe immune response, resulting in chemicals flooding your bloodstream, resulting in shock; your airways close and your blood pressure drops, and immediate medical attention is necessary. Why is epinephrine a life-saving drug?Epinephrine is so useful during a anaphylaxis crisis because it increases blood flow in veins, thus decreasing swelling in your airways. Epinephrine, a hormone that the body naturally produces, is known as adrenaline and is associated with our fight-or-flight response. This is because epinephrine plays a significant role in the contraction of muscles, the metabolism of sugar in the bloodstream, and a person’s feelings of awareness and fear. Epinephrine may also attach to receptors on smooth muscle cells, which control autonomic processes such as breathing. So, when epinephrine is administered using an EpiPen, an epinephrine auto-injector, to the upper thigh, the hormone binds to the smooth muscle cells, causing airway constriction to subside. The hormone also signals your body to pump more blood, relaxing muscles and returning breathing to normal; this subsides the significant symptoms of anaphylaxis shock and may save a person’s life. However, it is important to note that epinephrine is not a long-term medication for allergies, and should not be a substitute for allergy medications such as antihistamines.
By Sarina Thapar The terms “allergy” and “intolerance” sound similar and most people would say that they are synonymous; however, this is a common misconception. Food allergies and intolerances exhibit clear differences and require different types of treatment.
A food allergy is defined as a chronic condition in which exposure to a food triggers a damaging immune response. This response, called an allergic reaction, occurs because the immune system identifies these proteins as invaders in the body. The immune system overproduces antibodies called Immunoglobulin E (IgE) to attack the proteins, causing an allergic reaction. Food allergies can cause serious reactions by consuming or inhaling microscopic amounts of the offending food. Signs of an allergic reaction include hives, a swollen throat, and itching or tingling of the lips. Anaphylaxis is a serious allergic reaction that, if not treated immediately, can be fatal. In contrast, food intolerances are often less damaging because they involve the digestive system. In some cases, one is able to eat small amounts of the offending food without harmful effects. He or she may also be able to prevent an adverse reaction. For example, having a dairy allergy is sometimes confused with being lactose intolerant. Those who are lactose intolerant are able to drink lactose-free milk or take lactase enzyme pills to aid digestion. A food intolerance might make you feel uncomfortable or cause indigestion, but a food allergy has the potential to be life-threatening. Both food intolerances and allergies can cause nausea, stomach pains, excessive gas, and fatigue. This is why you should be aware of the effects that food has on your body. It is important to get tested for food allergies if you suspect a food is causing you harm. It is important to distinguish between food allergies and food intolerances in order to maintain good health and stay safe. By Samhitha Mupharaphu |
Details
Archives
May 2021
Categories |
Powered by
 Create your own unique website with customizable templates.
Create your own unique website with customizable templates.
 Create your own unique website with customizable templates.
Create your own unique website with customizable templates.



 RSS Feed
RSS Feed